Exp. No. 6 Isolation and identification of clinically important fungi: Candida sp., and Aspergillus sp.,
Isolation
and identification of clinically important fungi: Candida sp.,
Introduction
Candida are the members
of the normal flora of skin. More than 100 species are available in Candida.
Among these Candida albicans cause most of the human infections. The germ tube
test provides a simple, reliable and economical procedure for the presumptive
identification of Candida albicans. About 95% of the clinical isolates produce
germ tubes when incubated in serum at 35°C for 2.5-3 hours. A germ tube
represents the initiation of a hypha directly from the yeast cell. They have
parallel walls at their point of origin. Germ tube formation is influenced by
the medium inoculum size and temperature of incubation. Fresh normal pooled
human sera or a commercially available germ tube solution to be used as the
medium for the test. The inoculum should result in a very faintly turbid serum
suspension. Over-inoculation will inhibit the development of germ tubes.
Incubate in at 35°C-37°C for 2.5-3 hours.
Aim
To identify Candida albicans.
Materials and Methods
Wooden applicator
stick, Serum, Test tubes, Incubator, microscope, Culture of Candida albicans
on SDA medium
Procedure
· Using a Pasteur pipette, dispense 3 drops of fresh pooled human serum into the tubes. With a sterile wooden applicator stick, lightly touch a yeast colony and place the stick into the serum. Suspend the yeast in the serum. Discard the stick in a discard container. Incubate the tubes at 35°C for 2.5-3 hours. Placed a drop of the suspension on a clean microscopic slide. Placed a clean cover glass over the suspension and then examine it with a microscope using the low power objective. Use high power objective to confirm the presence or absence of germ tubes. Read control and record results.
Tube like outgrowth is
identified as germ tube. The given culture was found to be Candida albicans.
Introduction
Fungi are significant,
sometimes overlooked, human pathogens. Infection caused by the fungus ranges
from procedure includes Demonstration of fungi by microscopy, Identification
by culture, Detection of specific humoral mild to life threatening. Diagnosis is
based on a combination of clinical and laboratory investigations. Laboratory
response and Detection of fungal antigens and metabolites in body fluids.
Aim
To collect proper
specimen for the isolation of fungal pathogens and to perform fungal isolation
techniques.
Materials
and Methods
Czapek dox agar and
culture.
Procedure
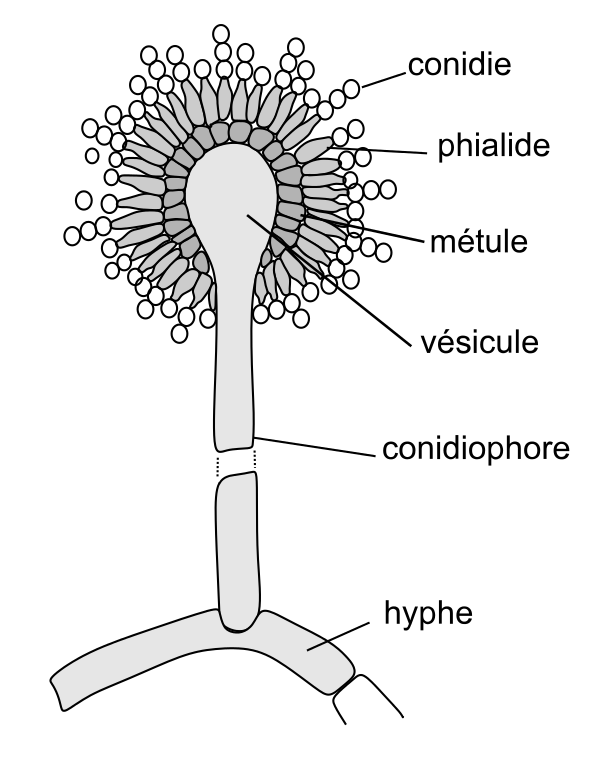
Fungal species may
sub cultured on different commercially available mycological media. On selective
and differential medium fungal species grown initially as white/multicolored
mycelium. Fruiting bodies / asexual are formed during growth, which is
considered as a selective character for identification. Conidium are usually identified by making use of any one of the following methods. Block
inoculation, Scarification are the subculture inoculation methods. Slide
culture technique, tease preparation and cellophane tape mount are used to
identify conidial structures. All these techniques use Lactophenol Cotton Blue
as a clarity stain for clear visualization of fungal elements. Size and shape
of the conidia will vary depends up on the genus. The following are different
types of conidia present in different fungal species.
Result
Fungal species can be
identified based on microscopic morphology and culture as Aspergillus sp.

Comments
Post a Comment